Geographic Variation in Diagnostic Ability and Quality of Care Metrics: A Case Study of Ankylosing Spondylitis and Low Back Pain
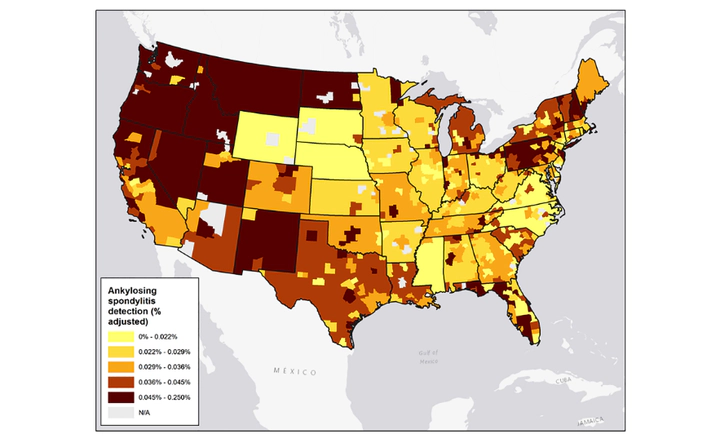 Image credit: Jinjoo Shim
Image credit: Jinjoo ShimAbstract
Studies examining geographic variation in care for low back pain often focus on process and outcome measures conditional on patient diagnosis but generally do not take into account a physician’s ability to diagnose the root cause of low back pain. In our case study, we used increased detection of ankylosing spondylitis—a relatively rare inflammatory back disease—as a proxy for diagnostic ability and measured the relationship between ankylosing spondylitis detection, potentially inappropriate low back pain care, and cost. Using 5 years of health insurance claims data, we found significant variation in ankylosing spondylitis detection across metropolitan statistical areas (MSAs), with 8.1% of the variation in detection explained by a region’s racial composition. Furthermore, low back pain patients in MSAs with higher ankylosing spondylitis detection had 7.9% lower use of corticosteroids, 9.0% lower use of opioids, and 8.2% lower pharmacy cost, compared with patients living in low-detection MSAs.