Erythropoiesis-Stimulating Agent Use After Changes in Medicare Reimbursement Policies
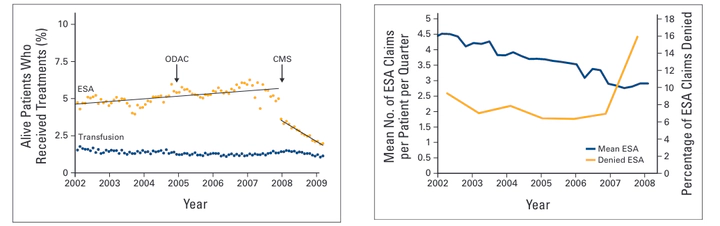 Image credit: Jinjoo Shim
Image credit: Jinjoo ShimAbstract
Since 2004, concerns about the safety of erythropoiesis-stimulating agents (ESAs) have resulted in label changes and restrictions on their use. We examined changes in ESA use and blood transfusions over time. The SEER-Medicare database was used to identify patients age ≥ 65 years with breast, lung, prostate, ovary, or colon cancer, diagnosed between 2000 and 2007, who had a chemotherapy claim after their cancer diagnosis. We calculated the mean number of ESA claims per patient per year. Follow-up claims were available through 2008. We used multivariable logistic regression models to analyze the association of ESA use and extended ESA use with clinical and demographic variables. Among 121,169 patients identified, 46,063 (38%) received an ESA. ESA use increased from 12.4% to 16.2% by 2006 and then decreased to 7.9% by 2008. Similarly, the mean number of ESA claims per patient decreased steadily over the entire timeframe. The annual percentage of patients undergoing transfusion remained relatively constant (9% to 10%). In a Cox proportional hazards time-dependent model, ESA use was positively associated with black race (odds ratio [OR], 1.11; 95% CI, 1.07 to 1.15), metropolitan location (OR, 1.17; 95% CI, 1.13 to 1.21), metastatic disease (OR, 1.39; 95% CI, 1.35 to 1.41), female sex (OR, 1.17; 95% CI, 1.14 to 1.20), > one comorbidity (OR, 1.29; 95% CI, 1.25 to 1.32), and tumor type. The number of denied claims increased over time. Our study demonstrated a rapid decline in the percentage of patients treated with ESAs after changes to reimbursement policy, but not after warnings about use. Reimbursement restrictions of other overused or off-label drugs may help reduce health care expenditures.